

These challenges have motivated innovation in ancillary technologies: formulation chemistry, protein engineering, glucose-sensing technologies and delivery devices. Indeed, glycaemic excursions outside the narrow blood glucose range classified as normoglycaemia (4.4–6.7 mmol/l) are frequent despite strict adherence to dietary and lifestyle recommendations. During a typical 24 h period, patients on insulin therapy often exhibit episodes of hyperglycaemia or hypoglycaemia, despite individualised dosing regimens and the broad use of engineered basal and rapid-acting insulin analogues.

Advances in diabetes technologies have been broadly motivated by the aim to link optimisation of IRT (including individualised glycaemic goals in type 2 diabetes ) and healthcare outcomes. Insulin replacement therapy (IRT) is essential for the treatment of type 1 diabetes mellitus and often required by patients with late-stage type 2 diabetes. Prospects are discussed for intrinsic glucose-responsive insulin analogues containing a reversible switch (regulating bioavailability or conformation) that can be activated by glucose at high concentrations. In each case, innovations in insulin chemistry and formulation may enhance clinical outcomes. Innovations span control algorithms for CGM-based insulin-delivery systems, glucose-responsive polymer matrices, bio-inspired design based on insulin’s conformational switch mechanism upon insulin receptor engagement, and glucose-responsive modifications of new insulin analogues. This review highlights three broad strategies to co-optimise mean glycaemic control and time in range: (1) coupling of continuous glucose monitoring (CGM) to delivery devices (algorithm-based ‘closed-loop’ systems) (2) glucose-responsive polymer encapsulation of insulin and (3) mechanism-based hormone modifications.
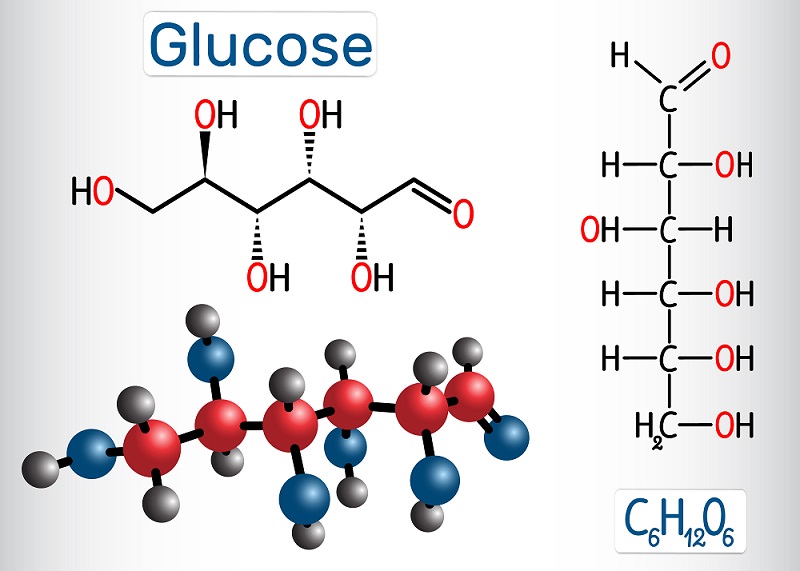
Such ‘smart’ systems or insulin analogues seek to provide hormonal activity proportional to blood glucose levels without external monitoring. To mitigate acute and chronic risks of such excursions, glucose-responsive insulin-delivery technologies have long been sought for clinical application in type 1 and long-standing type 2 diabetes mellitus. Insulin replacement therapy for diabetes mellitus seeks to minimise excursions in blood glucose concentration above or below the therapeutic range (hyper- or hypoglycaemia).


 0 kommentar(er)
0 kommentar(er)
